The next global pandemic is not going to be stopped by a wall, trade barriers, or a travel ban. A look at what has worked and what hasn’t as we face a new Ebola outbreak in Africa.
It sounds like it should be the beginning of a joke: A virus walks onto a plane… Only it’s not a joke. It’s how a global pandemic can start. One that could be far more immediate and deadly than our twin fears of climate change or nuclear proliferation.
The recent outbreak of Ebola in the Congo is a grim reminder not only of the 2014 West African outbreak, but of the much wider dangers of the global spread of infectious diseases — diseases that know no walls, no travel bans, and respond only to medical and political competence.
The Hill’s national correspondent Reid Wilson, in this week’s WhoWhatWhy podcast, talks to Jeff Schechtman about the very real dangers we face and how the incompetent handling of such a crisis could lead to loss of life on an unimaginable scale.
Wilson, the author of Epidemic: Ebola and the Global Scramble to Prevent the Next Killer Outbreak, takes us through the slowness of the global mobilization in 2014 and what we have since learned. It was a time when — as Wilson says — in parts of West Africa, it was easier to count survivors than count the dead.
Wilson explains how the World Health Organization (WHO) has learned how to better navigate global politics and local customs. As an example, 70 percent of those that had contact with dead bodies in 2014 contracted the disease; WHO learned that, in dealing with the dead, anthropology was as important as biology. In navigating behavior around the dead, respect had its own rules and customs in the developing world.
Wilson singles out Doctors Without Borders as the most heroic of the organizations that have been called upon in these global outbreaks.
We learn about the role of the Centers for Disease Control and Prevention (CDC) during the previous outbreak. It was an event that precipitated a major transformation of the CDC — one that resulted in the CDC sending about 1,400 people to Liberia during this recent outbreak. This was a drastic improvement over past efforts where only a few CDC field operatives were mobilized. Additionally, in 2014 the CDC only had four US facilities prepared to triage highly infectious diseases, such as Ebola. Today there are over 50, at least one in every state.
Even with all the progress and lessons of the the past four years, Wilson reminds us that a strategy for dealing with a rapidly spreading and deadly disease is only as good as the weakest link in the global public health system. That no matter how much the US may want to withdraw from the world, the public health systems in countries like Liberia, Guinea, and Sierra Leone matter to us all.
Wilson reports that what keeps public health professionals up at night is the fear of a disease with the lethality of Ebola, the prevalence and transmissibility of something like Zika — and one that develops enhancements for human-to-human transmission capability.
Some bird flu cases in China have already hinted at the possibility of these properties. These are diseases that could easily exceed the Ebola mortality rate of over 40 percent.
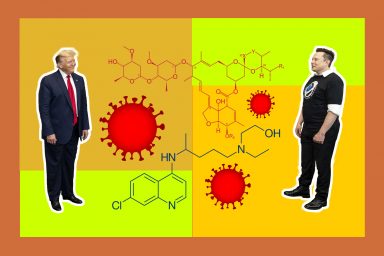
All of this is against the backdrop in the US of the Trump administration trying to claw back $250 million out of the Ebola supplemental funding bill, which was passed in 2014 and has been critical to the CDC efforts. Clearly we ignore global partnerships at our peril, especially as they involve the arena of public health. All the while the Chinese seem to be taking on greater and greater responsibility as part of their efforts to sit atop the world stage.
Click HERE to Download Mp3
Full Text Transcript:
As a service to our readers, we provide transcripts with our podcasts. We try to ensure that these transcripts do not include errors. However, due to time constraints, we are not always able to proofread them as closely as we would like. Should you spot any errors, we’d be grateful if you would notify us.
| Jeff Schechtman: | Welcome to Radio WhoWhatWhy. I’m Jeff Schechtman. No matter how much some may want to pull up the proverbial drawbridge and preach America first, the world is an interconnected place. The free flow of money around the globe, of jet travel and modern telecommunications, make the forces of globalization inevitable. And if those forces aren’t enough, the ability of disease to travel across the globe should be another reminder. |
| The fear that permeated all of us during the 2014-2015 Ebola outbreak in Africa is a grim and hopefully constant reminder. In fact, some argue that the greatest threat to the planet today, it’s not just climate change, or the threat of nuclear weapons, but the real threat of global pandemic. That’s our subject this week as we talk to my guest, Reid Wilson. | |
| Reid Wilson is a national correspondent for the Hill in Washington. He covers politics and public policy and elections. He has examined all sides of this issue of public health in his new book Epidemic: Ebola and the Global Scramble to Prevent the Next Killer Outbreak. And it is my pleasure to welcome Reid Wilson to Radio WhoWhatWhy. Reid, thanks so much for joining us. | |
| Reid Wilson: | Well thanks for having me. |
| Jeff Schechtman: | One of the things that’s remarkable about this story, and perhaps it shouldn’t be, but when we look at something like a global pandemic or the potential that the Ebola crisis had, how much of it gets caught up, how much of the attempt to deal with it gets caught up in politics, not just domestic politics, but global politics for that matter. |
| Reid Wilson: | Yeah. A lot of it does, and I think we can see that in evidence in this latest Ebola outbreak that’s taking place right now in the Democratic Republic of the Congo. We’ve seen the World Health Organization (WHO) race in there, but only after the invitation of the local health ministry, the health ministry of the DRC. And that’s really what happened in West Africa. |
| The World Health Organization is this global body that we all think of as the group that’s going to come and save us, but in fact, it is sort of the patron of its client states. And in the early days of the outbreak, there were tourism ministers in Liberia, Sierra Leone, and Guinea, the places that we’re talking about in terms of this outbreak, who were leery obviously of having the presence of Ebola in their country well known. | |
| These are desperately poor countries that were only just recovering from decades of civil war. And to have something like Ebola hit them, would diminish their standing, they thought, in the world hierarchy, and therefore they were a little leery about inviting the WHO in. So, the politics at play, they’re global, they’re national, and in a lot of cases they’re local. | |
| This virus hit a part of … it started in a part of Guinea and then spread over to rural Liberia and Sierra Leone that are far away from the capitals of each of these three countries. And there are centuries of mistrust between the local centralized governments, which are mostly made up of the descendants of American slaves. | |
| And the more rural areas that are dominated by tribes that had been there for thousands of years. So the distrust and the politics begins at the local level and it filters all the way up to these big global international bodies that we think are poised to save us. | |
| Jeff Schechtman: | And did the crisis in 2004, the Ebola crisis in 2014, 2015. Did that provide some kind of a cautionary tale to these countries in terms of how devastating it can be? |
| Reid Wilson: | Yeah, I think it did. And not just these countries but to the world at large. I say that WHO wasn’t entirely prepared to race in and contain this virus. As a matter of fact, a lot of it was left up to the American Centers for Disease Control and Prevention (CDC) to go in, and I should say, groups from across the world, the United Kingdom, and some NGOs there, France, Italy, even Germany and Denmark did a lot to prevent the virus from spreading further. |
| But it certainly had a cautionary note because the big international systems that we thought were in place to fight back against a pandemic simply weren’t there and they weren’t able to do their job. The WHO had no list of doctors who could volunteer at the drop of a hat or contractors who could fly in pallets of body bags and chlorine solution to spray everything and kill the virus. | |
| In the wake of the outbreak, WHO has undergone a remarkable round of self-flagellation really and reorganized itself into an organization that’s much more able to respond to one of these outbreaks. And again, we’re seeing that now in the Democratic Republic of the Congo, the director general of the WHO was in the hot zone itself, just days after this latest outbreak was confirmed, essentially showing that, hey, the WHO is now an organization that is able to respond to something like this. | |
| And of course, the next big one that we’re talking about, it’s not really going to be Ebola. Ebola is difficult to spread between humans. You actually have to touch, you know, blood or guts to get it yourself. The next one is going to be something that spreads easily among humans and has a highly fatality. It’s probably going to be something like a flu. | |
| So, all right, WHO is good at responding to a virus like Ebola, but what about the next SARS? What about the next bird flu that comes out of some bird market in China or something like that. Will they be prepared to respond to something at that scale? That’s something we don’t know yet. | |
| Jeff Schechtman: | And when we look at the totality of this, what role did other NGOs play in this crisis and what role might they play going forward today? Groups like Doctors Without Borders. |
| Reid Wilson: | Yeah. Doctors without Borders is … they’re the real heroes of this story. This is an amazing organization that goes into places all over the world to respond to … whether it’s a health crisis like the Ebola outbreak or a war or a famine or something like that. One of the Doctors Without Borders volunteers who I spoke to for this book is a guy named Craig Spencer. |
| He got the Ebola virus himself. He’s a doctor up in New York. He just emailed me the other day and said he was on his way to a rescue boat in the Mediterranean where he is going to help pickup migrants who were put on these little dinghies, overcrowded little dinghies in Libya and sent over to Italy. So, a really amazing organization that does incredible work. | |
| And they were the ones who really stepped up in creating Ebola treatment units. The places where people would actually be treated. They were among the first into the fight, they were the ones who were able to sort of begin treating patients and figuring out how to bring the mortality rate of Ebola down from 80 or 90 percent to 40 or 50. | |
| Which is still an amazingly high mortality rate, but of course you’re saving a lot more people that way. Other NGOs are groups like Global Communities, it’s an American based NGO that’s operated in Liberia for years. They operated sanitation systems and taught people about the links between open sanitation and cholera. | |
| Well, they were able to transform their teams that would go village to village and dig these safe latrines and things like that into burial teams, teams that were tasked with taking a body, if there was somebody who had died from the Ebola virus, and giving it a safe burial because what they found out was about 70 percent of all the Ebola transmissions were coming as people came into contact with dead bodies. | |
| This is … by the way, another lesson from the Ebola outbreak. One thing we learned was that anthropology matters as much as the hard sciences. So when you’re burying a body, you can’t just take somebody’s loved one and throw it in a grave. You have to show respect. | |
| You have to talk to the family about who this deceased person was, what they’re going to do in the afterlife, and then pick up the body in full view of the family, disinfect it, bury it safely, all in view of a family that is obviously mourning because they just lost their loved one. And a family that demands actual respect for the deceased. | |
| So the cultural traditions there were a big, huge lesson that a group like Global Communities was able to impart. They’re also, by the way, I should point out faith groups that played a huge role in a lot of places. In Sierra Leone groups like World Vision, you’ve seen them because they’re the group that runs TV ads that say, “Hey, thirty cents a day or something, can save a kid’s life.” | |
| Well they had something like 56,000 sponsored kids in Sierra Leone. They worked with faith leaders, both Christian and Muslim. And this is the part of the story that I absolutely love. The Muslim, Imams and the Christian ministers standing side by side and talking to their congregations about how to stay safe. | |
| World Vision, ended up spreading that message and then becoming a system of burial teams that are sending out a group of burial teams themselves. And of those 56,000 kids that they have sponsored, not a single one in Sierra Leone, got sick. | |
| Jeff Schechtman: | Talk a little bit about the global mobilization that took place then, and what we learned from it with respect to its spreading beyond the original hot zone. |
| Reid Wilson: | Right. The global mobilization was pretty slow. The very first person who got the Ebola virus was a two-year-old boy named Emile in a tiny village in Meliandou, which is up in the mountains of rural Guinea. He got it in December of 2013. |
| The World Health Organization didn’t know that there was anything wrong or the local health ministries too, didn’t know anything was wrong until about late January when they went into this area and they thought they were looking at a cholera epidemic. A cholera outbreak, because they didn’t know to look for Ebola. Ebola is not endemic to this part of Africa. | |
| It’s endemic to the Congo river basin, which is effectively 2,500 miles away. I mean, it’s basically as far away as you and I are right now, I’m in Washington DC. So they didn’t know what they were looking at. A few months later Doctors Without Borders got involved and the WHO got some samples, they both tested those samples at about the same time in late March of 2014 and finally realized they had Ebola. | |
| The first teams from Doctors Without Borders, WHO, started arriving in March, the first teams from the Centers for Disease Control and Prevention arrived in April. But the full scale response didn’t really start until August, when people realized that there was a real serious problem here. And the reason is because West Africa is a much different place than the Congo River Basin. | |
| The Congo River Basin, it’s difficult to travel. You’ve basically got to go up and down the river if you’re even on the river. So if this breaks out in a remote village, it’s going to infect the people in that village, and probably nobody else. West Africa is a much more trade based, sort of transient region, where people routinely cross borders and travel to the capital to trade. | |
| To bring their goods from one city to another. And that meant that the virus had a lot more vectors to get out of this tiny little village of Meliandou, and into first surrounding towns and then across borders and then to these big mega capitals that have a million people and some of the most densely packed slums in the world. | |
| So, the spread of the virus … it happened because we are a transient … that region is a transient society. And I would say, that’s how the world is these days. We travel much more now than we ever have before. The booming middle classes of Africa and Asia are traveling to Europe and the Middle East and the United States. | |
| And of course the booming middle class in United States is traveling to all of these other places too. This is a big thing. I’m sorry for the tangent, but every time somebody says, “Well, if we just put up a wall, and banned travel.” It’s like, “No, Americans like to travel too and you’re not going to keep Americans overseas, if they come down with something like this.” | |
| So the bottom line is we are becoming an increasingly interconnected world and that is how any of these viruses can spread further. | |
| Jeff Schechtman: | It seems like the other part of that problem, to just stay on that point for a moment, it’s not only are we increasingly interconnected, but the difference even from four years ago. The initial Ebola crisis, there’s so much more nativism at play today. So much more desire to close off borders and the danger that that poses today? |
| Reid Wilson: | Yeah, I think so. And the notion of closing off borders is … viruses don’t know anything about international borders, right? They’re not going to respect a border. Every pandemic that we know of has spread regardless of what kinds of travel bans we place. And by the way, when it came to West Africa, there were a lot of people in Congress who were calling for travel bans from West Africa. |
| Anybody who’d been there, they didn’t want them to come to the United States. That has a side effect of keeping people who want to go help out of the hot zone. So basically, if any American Doctors Without Borders volunteer or CDC official or even members of the US Army, wanting to go help in West Africa, they would have been prohibited from traveling back to the United States. | |
| You don’t want to do that, because that robs you of the people who were going to solve this crisis. As it happened, after United States sent 3,000 American troops over there, not a single one of whom got sick, when they came back, they did spend 21 days in quarantine. I talked to a few of who did this, that it was the most boring 21 days of their entire lives. | |
| Jeff Schechtman: | Talk a little bit about the role of the CDC and the US military in this particular crisis. |
| Reid Wilson: | Right. So the CDC really underwent a massive transformation during this outbreak. This is an agency that used to pat itself on the back when they sent a dozen or two dozen people out into the field to combat some kind of viral outbreak. In the course of this outbreak, they deployed more than 1,400 people, sometimes two or three times into the hot zone. |
| And they focused their efforts mainly in Liberia, which has the closest relationship with the United States. Sierra Leone as a very close relationship with the UK. Guinea has a very close relationship with France. So they sort of divided up the responsibility that way, but there were CDC teams doing literally everything in the outbreak. | |
| Some people organize the response, they sort of coordinated the entire response at emergency operation centers that were funded by people like Paul Allen and the CDC foundation. They operated the response here at home. They prepared hospitals across the country to get ready for an Ebola patient to walk through the door. | |
| Before this outbreak, there were only four facilities in the US that could have treated somebody with Ebola in isolation. Today, there are more than 50, one in every state. And in some states, several. In West Africa, they handled contract tracing, which is making sure that you know if somebody comes down with Ebola, you track everybody that they’ve come into contact with because those are the people who are now most likely to get Ebola themselves, and they even did things like border control. | |
| The borders between these three countries and other countries were drawn a century and a half ago by cartographers in Paris and London. They don’t make a lot of sense to the tribes who actually live there. So the borders are very porous. Well, you’ve got to track who’s going back and forth so you can track the spread of the virus and therefore understand how much you sort of have to respond in certain areas. So they even handle border control. | |
| Jeff Schechtman: | What changed if anything once the virus made its way to New York? |
| Reid Wilson: | Well, the virus first came to the United States in October when a man named Thomas Eric Duncan boarded a flight in Liberia and traveled to Dallas. That was really a wake-up call because it showed that travel happens and that people are coming across borders regardless of whether or not you implement some kind of flight banner or something like that. |
| A few weeks later, another … well a few months later, another volunteer, a doctor from Doctors Without Borders, Craig Spencer, got back to New York and, a common theme in the people who served over there over in West Africa, and then came back, is depression. Because this was an outbreak where basically it was easier to count the survivors than it was to count those who died because there were just fewer survivors. | |
| It was a terrifying moment to be actually on the ground in West Africa. And so when people came back, they suffered through a lot of depression. Craig Spencer felt that same way. And then a few days later he started to feel these aches and pains. He sort of woke up one morning and realized something wasn’t right. He was exhausted, he was sweating all over the place. His temperature was starting to rise. | |
| And then that was a moment when Americans realized that this virus could get to the United States. And it was also a moment when another client of … sort of a client for the US government, if you will, American hospitals started paying a lot of attention. This was before there were a ton of hospitals that could handle an isolation patient. | |
| And so the hospital that he went to, he went to Bellevue Hospital in New York, ended up sort of being the test case and a lot of people were … a lot of hospitals were super nervous about treating an Ebola patient and being seen as a place where somebody with Ebola might go because the hospital in Dallas, that treated Thomas Eric Duncan, had lost so much business afterwards. | |
| People didn’t want to go to a place that had treated an Ebola patient. So it was a moment when American hospitals were deciding whether or not to essentially build their capacity to treat an Ebola patient. And Bellevue itself got the support of the Centers for Disease Control and Prevention, which by the way, the head at the time, Thomas Frieden, had been the public health commissioner of New York City. | |
| So he knew the hospital’s pretty well. And the CDC, and the US government, really tried to show hospitals around the country, if you get an Ebola patient, we will have your back. We will give you all kinds of support. And that mattered a lot. That sort of incentivized a whole bunch of hospitals to get ready effectively and to prepare for the next Ebola crisis. | |
| So that moment in New York was an important one because it helped prepare hospitals in every other state to get ready for the next pandemic, if it were to come. | |
| Jeff Schechtman: | If the event were to happen today, what might be different? |
| Reid Wilson: | I think, well, we’re seeing the event happening today and I think a couple of things are different. This outbreak in West Africa hit a small … I’m sorry, this outbreak in the Democratic Republic of the Congo that’s going on right now, started in a small village. It moved to a village near the Congo river, and then terrifyingly enough, it hit a city of about a million people that’s actually on the Congo river. |
| Now, that’s scary because people can travel up river to one foreign capital and downriver to three foreign capitals, including Kinshasa, which is a city of like 12 million people. So there’s a little terrifying moment. The difference is, the international response happened almost immediately in this case. It took about four months in West Africa to identify the Ebola virus. | |
| In this case, it probably took about a month. They’re still looking for the very first case, what we call the index case, but within days of the first acknowledgement that the Ebola virus had broken out, there were teams on the ground and we now have a vaccine for the Ebola virus. And, so there have been about 1200 people in these three cities that have had contact with Ebola patients that have been given the vaccine. | |
| Frontline healthcare workers have been given the vaccine. Hopefully it ends up working, but we won’t actually know that it does until about two months from now when the sort of incubation periods have ended in these three communities. But the response has been amazingly fast. I talked to this man named Pierre Roland, he’s the CDCs like chief Ebola expert. | |
| And he was getting on a plane the next day, two days after this declaration of an outbreak had taken place to go, and to go experience what … to go see what was actually happening in the DRC and to deploy themselves. The CDC maintains an office in Kinshasa. They have deployed up to the hot zone themselves to help with the response, and groups like Doctors Without Borders. | |
| Doctors Without Borders opened three Ebola treatment units in the space of about a week, which is really impressive in terms of speed. It takes a lot to open a facility like that and they now have sort of demonstrated that they’re the first line responders who are able to open a place like that in just a blink of an eye. | |
| Jeff Schechtman: | Of course, the other danger and there’s familiarity with Ebola at this point is some other disease spreading that we’re less familiar with at this point. |
| Reid Wilson: | Yeah, that’s right. The World Health Organization every year puts together a list of diseases that need to be given research priority. And so it starts with AIDs and Ebola and Lassa, Hemorrhagic Fever, and things like that. But they have just recently added another one to the list that they’re calling “Disease X” and Disease X is the unknown. |
| And it’s the one that could spread … look the thing that keeps public health officials up at night is something that has the lethality of Ebola, the transmissibility and the prevalence of something like Zika. Zika is a virus that if you or I get it, it’s not going to do anything to us. It only basically affects fetuses. | |
| However, it is much more easily transmissible and much more widely transmissible because its carrier, these mosquitoes are basically everywhere. Blame climate change for that one. The fact is that if you combine the spreadable disease like Zika, and a lethal disease like Ebola, and then add in human-to-human transmission, which is not something that the Zika can do, that’s what keeps doctors up at night. | |
| And that means it’s probably a flu. The next big thing … you know, here we are in 2018, 100 years after the Spanish Flu killed something like 50 to 100 million people around the globe and the Spanish Flu had a mortality rate of about 2.5 percent. Ebola at the moment in West Africa had a mortality rate of somewhere north of 40 percent. | |
| So, all right, if you get something of the scale of Ebola with the spread of the Spanish Flu, that’s going to scare the public health. That’s the next Disease X effectively. And not to scare everybody or all your listeners, but there is a flu in China right now that’s not terribly transmissible between people, but it’s broken out a few times in some bird markets that has a mortality rate of 35 to 40 percent. | |
| So, that’s pretty scary. That’s what doctors are watching right now. And then again, it’s Disease X, even if they get a handle on this particular flu, there might be another one that comes up. | |
| Jeff Schechtman: | And practically speaking, what is the need for more funding globally to deal with all of this? |
| Reid Wilson: | So the need is severe. Think about it like this, the global public health system as we saw in West Africa, a virus can get on a plane and it has gotten on a plane several times both in previous outbreaks, and in this outbreak. Planes traveling to Europe, planes traveling to Nigeria, planes traveling to the United States. The global public health system is only as strong as its weakest link. |
| And there are a lot of very weak links, especially in places like Sub-Saharan Africa. When you think about Liberia, Guinea, and Sierra Leone, the GDP of Liberia is 1% of what it is here in the United States. They don’t spend a lot of money on public health. Death is not uncommon in West Africa. And that is just sort of a fact of life, whether it’s Cholera, or Lassa, or Ebola, or something else like that. | |
| Because the world is becoming so interconnected, the health systems in Liberia matter to the United States, and matter to Europe, and matter to any one of us who live in this globalized society. I mean, you want to go lock yourself away in a cabin in the mountains, great, good for you, but that’s not how the rest of us live. | |
| And therefore without sort of bolstering this public health spending in places like Sierra Leone, Guinea, West Africa, and Congo, then we’re going to see more viruses spreading more widely across the rest of the world. | |
| Jeff Schechtman: | What about spending here in the US? Places like CDC and also in terms of looking at the broader coordination of this through interagency actions in Washington? |
| Reid Wilson: | Yeah. And that has happened a lot more. It’s interesting, in talking to a lot of the people who responded, they all said that the humanitarian responders, the people who respond to earthquakes, or floods, or tornadoes, or things like that, and the virus responders, the CDC, had always kind of viewed each other with suspicion. They didn’t get along, they didn’t talk much. |
| They didn’t have to. After this, the two groups sort of headlined by the CDC and USAID, the Agency for International Development, developed this really close working relationship. They realized, we don’t have to have this wall, this is sort of an artificial wall between two kinds of responds that doesn’t make a lot of sense. | |
| So they ended up tearing down that wall, operating a very close working relationship, and now they’re both sort of asking for the funding that they need to spend less here in the United States and more elsewhere. More around the rest of the world, so that they can engage in this disease surveillance. So, that they can identify the next Disease X that pops up. | |
| One thing that’s a little troubling right now is, remember the Ebola supplemental bill. The bill that Congress passed to deal with this Ebola crisis. That money is running out. And as a matter of fact, the Trump administration has proposed clawing back about $250 million from that supplemental bill, and saving the money effectively. | |
| Well, that was money that was going to be spent on bolstering public health systems in some other countries. And at the moment the CDC operates in 49 countries around the world where they do this sort of disease surveillance and keep a lookout for the next killer virus. When this money runs out, they’re going to have to cut back on 39 of those 49 countries. | |
| They only continue to operate in 10. So if we don’t fund CDC and USAID to the appropriate levels, that makes the rest of the global public health system more tenuous and, not as able to respond to the next disease and in turn, that makes all of us less safe. | |
| Jeff Schechtman: | And where does Western Europe fit into this equation then? |
| Reid Wilson: | Well, they … especially UK, have done a … well, just as much as the American CDC has, the UKs version of it is called UKFID, I think it is, something like that. There’s also the Welcome Trust in the UK. As I said, you know, the German government, the French government, the Italian government, the Danish government, all sent aid. |
| And in some cases like the Danish government paid for little like playing cards that talked about the danger of Ebola, these sort of … you know, it sounds like a tchotchke, but hey, that’s the way you communicate with people in rural villages who don’t have a radio to listen in or, a television or something like that. | |
| So all of these governments in Western Europe chipped in quite significantly, and again, they’ve done so in this outbreak in the Democratic Republic of Congo, that’s going on right now. The US government has given about $5 million to respond to this virus. Germany has given about … I think it was a million pounds … the last time I saw it, or a million euros. | |
| The UK government has chipped in … several different branches of the UK government have chipped in money. So the global response is not just Americans, it is also Europeans and increasingly by the way the Chinese are getting into the game. The Chinese have a version of the Centers for Disease Control and Prevention. | |
| They’ve learned a lot from the US and they’re trying to be more, sort of a more of a presence on the global stage, not just in terms of taking over the South China Sea or, raiding Africa of its rare minerals but also of trying to do something on the humanitarian side. | |
| Jeff Schechtman: | And they have a huge presence in Africa right now. |
| Reid Wilson: | That’s right, they do. In all parts of Africa from West Africa where they’re mining for diamonds, to down in Namibia where they’re mining for rare earth minerals and places like that. So it’s pretty remarkable how the Chinese have expanded, but in doing so, you know, the Obama Administration really tried to get the Chinese to understand that you have to sort of take on the responsibility of being a global player, and that means helping to respond in a case like this. And the Chinese did so, and in impressive fashion. |
| Jeff Schechtman: | Reid Wilson, the book is Epidemic: Ebola and the Global Scramble to Prevent the Next Killer Outbreak. Reid, I thank you so much for spending time with us. |
| Reid Wilson: | Okay, thanks a lot. It was really a lot of fun. |
| Jeff Schechtman: | Thank you. And thank you for listening and for joining us here on Radio WhoWhatWhy. I hope you join us next week for another Radio WhoWhatWhy podcast. I’m Jeff Schechtman. If you liked this podcast, please feel free to share and help others find it, by rating and reviewing it on iTunes. You can also support this podcast and all the work we do by going to WhoWhatWhy.org/donate. |
Related front page panorama photo credit: Adapted by WhoWhatWhy from plane (Andrew Nash / Flickr – CC BY-SA 2.0).